A group of 103 House members have not only added voices of support to the proposed nursing home staffing rule, they also want the mandated number of nurse hours per patient day inflated to 4.2 — a 40% increase over the proposal.
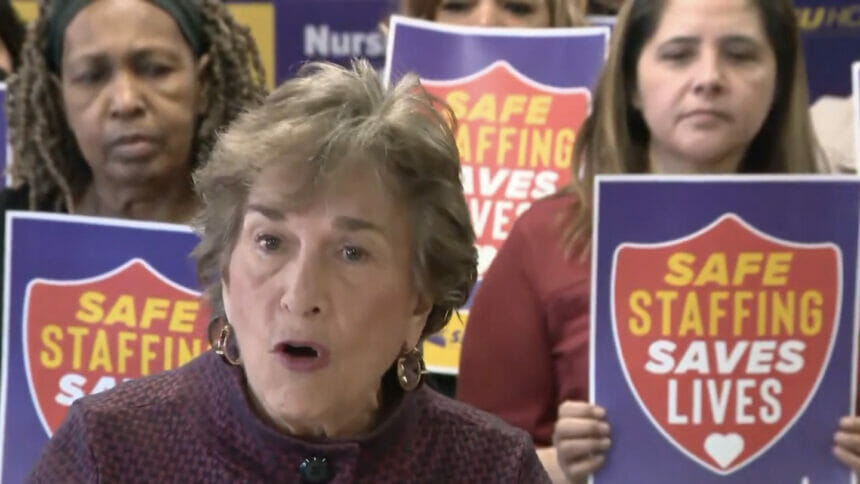
The lawmakers — led by Lloyd Doggett (D-TX), the ranking member of the House Ways & Means Health Subcommittee, and Jan Schakowsky (D-IL), of the House Energy & Commerce Committee (pictured) — sent a letter to President Joe Biden outlining their wishes Monday.
The Centers for Medicare & Medicaid Services left licensed practical nurses out of the proposed limits, which the letter signers worried would incentivize providers to eliminate LPN positions to meet other requirements.
“All levels of care are vital to ensuring quality care in nursing homes,” the letter stated, “and CMS’s final rule should reflect that reality.”
Their proposed solution was adding a 1.4 hours per resident day (HPRD) minimum to the mandate for LPNs. This suggestion is similar to proposals by groups of pro-mandate state attorneys general and US senators made in open letters Monday and Tuesday.
Phase in quicker, more gradually
The group of representatives also critiqued the timing of the proposed staffing rule.
“We urge CMS to phase in minimum staffing requirements rather than an abrupt, distant implementation date,” they wrote.
The letter expressed concern that such abrupt timing windows would incentivize policies that lead to negative outcomes, such as operators postponing recruitment until deadlines have nearly arrived.
The lawmakers also proposed that adding a more gradual series of deadlines to the new staffing requirements would smooth the transition and, “ensure residents and workers benefit from some improvement prior to the respective 3-year and 5-year final implementation dates.”
Smaller, more frequent goals would better position facilities to meet legal requirements on time, they added.
Stronger pay transparency urged
The group’s final major concerns regard staff compensation and working conditions, and with transparency of how facilities are using Medicare and Medicaid payments.
“While nursing homes may be chronically understaffed,” the representatives wrote, “this is not necessarily due to a shortage of qualified workers. Staff have been leaving nursing homes in droves, citing poor wages and benefits, dangerous working conditions, burnout, and little respect for their work.”
The representatives expressed concern that nursing assistants’ real wages declined in for-profit nursing homes in 2020 to 2021, despite payments from the Provider Relief Fund and continued profitability for many such facilities.
The group wrote in support of another proposed CMS rule requiring nursing homes to disclose their use of Medicaid payments for care worker and support staff compensation. They also suggested that this requirement be extended to Medicare. Finally, they suggested that nursing homes should be required to disclose the percentage of their total income used for worker compensation.
Opponents of the mandate have criticized the rule’s lack of additional funding for already-struggling nursing homes. In apparent response, the representatives claim these added transparency requirements would provide the government with needed information to decide whether additional payments are necessary to meet staffing and wage needs.



