
The Centers for Medicare & Medicaid Services, through its consumer‐facing website, has made additional nursing home staffing data available. Doing so during a public health emergency, when the industry is in an unprecedented staffing crisis, seems a bit tone deaf.
Nevertheless, the addition presents an opportunity to better understand a nursing home’s pathway to improvement.
A stable organization provides a desirable environment within which to give and receive care. We see these new data and resulting metrics as just some of the artifacts of an organization’s stability. Do staff, residents and families have a sense of confidence, security and optimism even in trying times like these? With this confidence, all stakeholders can act rationally and adapt effectively as challenges emerge.
Care Compare now includes the following metrics, all of which are derived from federal PBJ submissions:
- Total number of nurse staff hours per resident per day on the weekend
- Registered nurse hours per resident per day on the weekend
- Total nursing staff turnover
- Registered nurse turnover
- Number of administrators who have left the nursing home
You can read more about these metrics here.
From these new data points, we created measures that point to organizational stability. These measures are defined as:
- Staffing consistency (in staffing ratios between weekday and weekend). The idea here is that nursing staff ratios should be relatively the same across all days of the week (two variables).
- Staff turnover. The lower the turnover, the more stable the nursing home (three variables).
With these measures defined, we next excluded any nursing home that had missing data or was an extreme outlier (like the nursing home that reported 52 administrators had turned over within 12 months). These exclusions do make you wonder about the integrity of the data. But I digress.
Of the 15,238 nursing homes, 10,462 (69%) were included in the analysis. We used a statistical procedure called cluster analysis to group nursing homes into cohorts based on their stability profile. Next, we profiled the nursing homes in each cohort to determine if nursing home stability was associated with different (independent) performance outcomes, which are discussed below.
Through cluster analysis, we placed each nursing home into one of three cohorts:
- Unstable (38% of nursing homes): These nursing homes had the most variation in staffing patterns and the highest staff turnover.
- Somewhat stable (21% of nursing homes): These nursing homes had unremarkable staffing patterns and staff turnover.
- Stable (41% of nursing homes): These nursing homes had the most consistency in staffing patterns and low staff turnover.
There is a positive association between nursing home stability and overall Five‐Star rating
The more stable a nursing home, the better its overall Five‐Star rating tends to be:
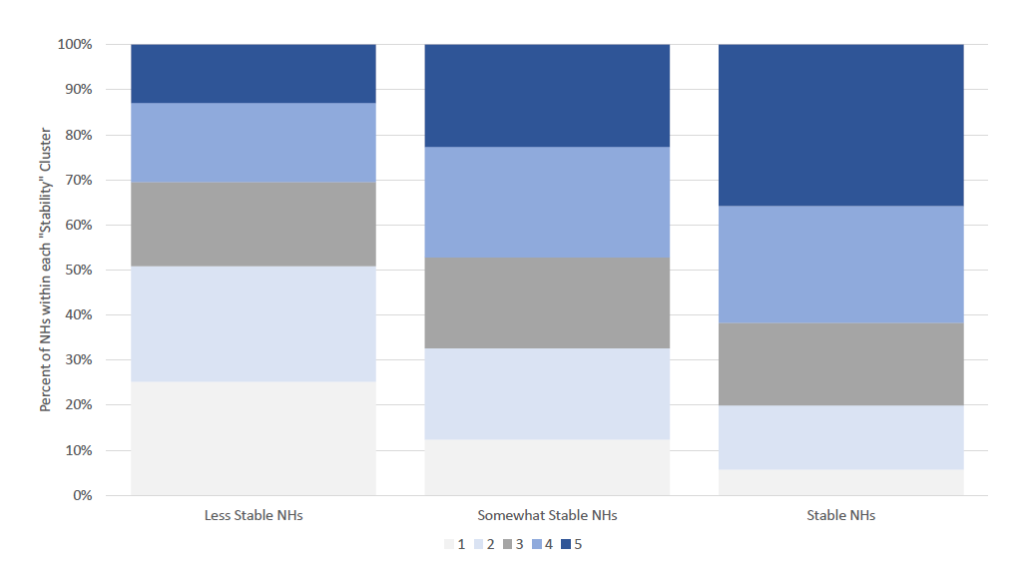
(Remember that the new data metrics are not currently part of Five‐Star, but they will be by July 2022.)
There is an inverse relationship between nursing home stability and key CMS measures such as SFF and the Abuse Icon
The more stable a nursing home, the less likely it is to land on the SFF or SFF candidate list:

The more stable a nursing home, the less likely it is to be assigned an Abuse Icon:
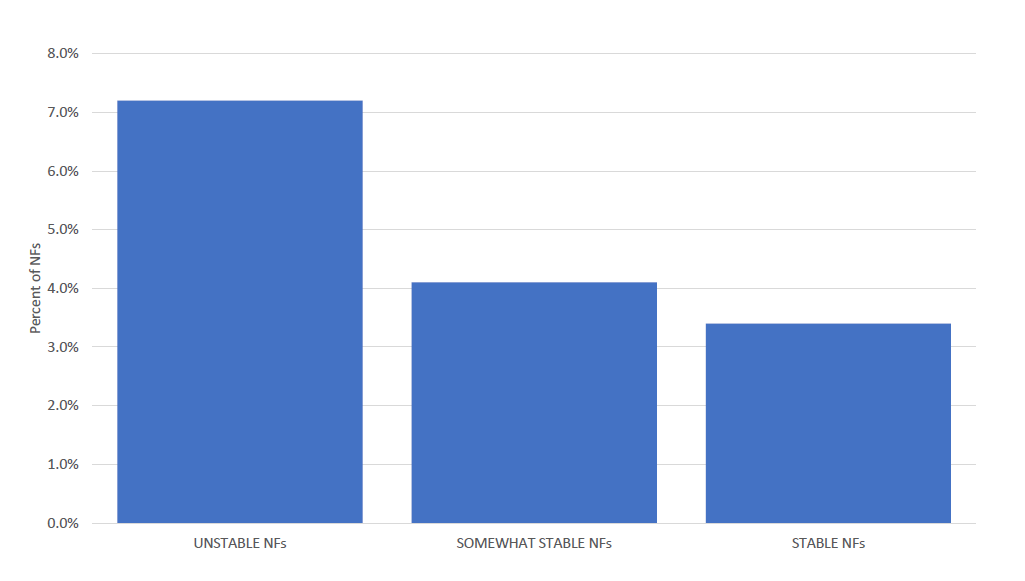
Doesn’t this make sense? If a nursing home has low turnover and staffing consistency, one could speculate it is providing consistent quality care.
Staffing is key to success, and unfortunately the most difficult to ascertain. Availability of staffing varies dramatically by state and county, but currently, all staffing metrics use national averages as reference points, rendering them insensitive to local influences and state‐level staffing requirements.
Hopefully, when the new data metrics are added to Five‐Star, CMS will place them in the context of each nursing home’s local operating environment. However, don’t wait. Look at your data now. Do they make sense to you? Are they accurate? Do they offer any insights into your nursing home’s operational stability?
Steven Littlehale is a gerontological clinical nurse specialist and chief innovation officer at Zimmet Healthcare Services Group.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.




