The Centers for Medicare & Medicaid Services late Friday announced that it will begin posting nursing home staff turnover rates and weekend staffing levels on the consumer-facing Medicare Care Compare site this month.
The same information will then be incorporated into the public Five-Staring rating system in July. The moves intensify pressure on providers that are facing a historic workforce shortage with no clear end in sight.
“Staffing in nursing homes has a substantial impact on the quality of care and outcomes residents experience,” CMS said in a memo announcing its decision to add the turnover rates and weekend levels to staffing averages that have been included for a decade.
The additional information “further enhances the information available to consumers, residents, and families to help support their healthcare decisions and incentivizes quality improvement among nursing homes,” the agency said.
Researchers have long associated nursing home staff turnover with lower star ratings and, increasingly, poor resident outcomes and infection control issues.
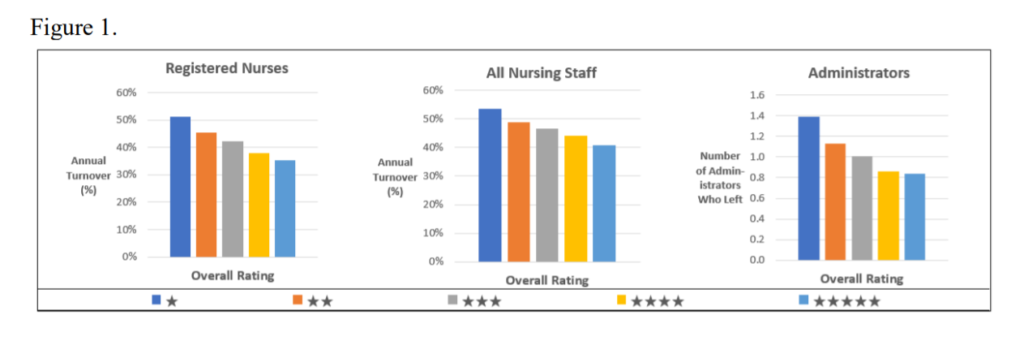
A national analysis published in Health Affairs early last year also found turnover to be much more prevalent than previously believed. Staggering mean turnover rates included 140.7% among registered nurses, 129.1% for certified nursing aides and 114.1% among licensed practical nurses.
“The publication of these statistics (by CMS) has been a long time coming,” said UCLA health economics assistant professor Ashvin Gandhi, who co-authored the Health Affairs paper with Harvard professor David Grabowski. Gandhi noted the Affordable Care Act set statutory requirements for the publication of such data, a move the researchers backed after their groundbreaking study.
“The pandemic has really turned pre-existing staffing problems in the industry into a full-blown crisis,” Gandhi told McKnight’s Sunday. “It’s probably more important than ever to make as much information available as possible.”
CMS noted in the memo some ways lowering turnover could help residents.
“Facilities with lower nurse turnover may have more staff that are familiar with each resident’s condition and may therefore be more able to identify a resident’s change in condition sooner,” the memo said. “In doing so, the facility may be able to implement an intervention to avoid an adverse event, such as a fall, acute infection, or hospitalization, which are indicators of quality.”
Administrators in focus
While much of the focus has been on nurse turnover in the industry, CMS also will draw attention to changes in administrative leadership. All facilities must report the percent of RN staff, the percent of total nurse staff and the number of administrators that have left in the last year.
CMS noted that reduced administrator turnover can provide “leadership stability” direction and may help staff “provide care more consistently or effectively to residents.”
“There is an old saying, ‘A fish stinks at the head,’ and if administration is unsatisfied and unstable, that will always lead the entire organization down the same path,” Melissa Brown, OT, chief operating officer of Gravity Healthcare Consulting, told McKnight’s Saturday.

“Learning how to and executing effective staff retention strategies will be more vital than ever,” she added. “Moving forward with business as usual will be a recipe for disaster. Staffing challenges are harder than ever before. … If providers don’t make deep, meaningful changes, it will come to haunt them in their Qualify Measures and on Care Compare.”
Historic struggle
The reporting announcement comes as providers across the country are clamoring for financial help and pushing back against new staffing legislation, arguing that they don’t have enough applicants to fill current jobs, much less add positions or afford enticements for hard-to-fill shifts.
Many are relying significantly on agency staff to plug holes in all kinds of positions. Some 420,000 nursing home workers have left the industry since February 2020, according to the Bureau of Labor.
“It is going to be critical to invest in the search process, the onboarding process, and continuing to invest in each individual employee to get the best associates and then retain them,” Brown said. “It won’t be enough to just fill an open staffing slot with agency. That has never been a good model based upon the care outcomes when a lot of agency staffing is used.”
She said the industry’s current reliance on agency staffing may be one reason CMS announced its somewhat unexpected move now.
She added that from a technical standpoint, it will be critical for nursing home recordkeepers to link their employees in the Payroll-Based Journal system any time they change employee identifiers to avoid inaccurately demonstrating increased turnover.
Weekend scrutiny detailed
Both CMS and the Health and Human Services Office of Inspector General have previously raised issues about weekend staffing. In August 2020, the OIG recommended CMS explore ways to provide consumers with additional information on nursing homes’ daily staffing levels and variability, such as how nursing homes’ weekend staffing compares to that of other nursing homes with the same staffing star rating.
In response to that and an April 2021 OIG report noting staffing variability during the pandemic, CMS will begin posting data on the level of weekend RN and total nurse staffing for all nursing homes on Care Compare. It will base turnover calculations of the average number of RN and total nurse hours worked per resident per day on weekends.
The goal, the agency said, is to encourage facilities to increase nurse staffing on weekends.
Technical specifications for weekend staffing and staff turnover measures will be included in the Five Star Rating System Technical Users’ Guide on Jan. 14, and employee-level data will be posted in the PBJ section of data.cms.gov on Jan. 26.

Of course, all that increased visibility into operations is likely to put additional pressure on providers.
“Residents and regulators will now be able to assess whether a facility is doing a good job retaining their staff,” Gandhi said. “Correspondingly, it’s likely that residents are going to prefer facilities with lower turnover, and we’ve even heard from some state regulators that they’re hoping to set higher Medicaid reimbursement rates for facilities with lower turnover. Facilities that want to improve their retention will need to better address the needs of their staff. It will be interesting to see how providers try to accomplish this. The obvious is to increase wages and benefits for tenured staff.”




